About the Children's National - NIAID Partnership
In 2017, The National Institute of Allergy and Infectious Diseases (NIAID) and Children’s National Hospital launched a clinical research partnership devoted to protecting and advancing the health of children with allergic, immunologic, auto-inflammatory, and infectious disease through collaborative research and education. This strategic and novel alliance is supported through the CTSI-CN. The partnership, co-led by H. Clifford Lane, M.D., Deputy Director for Clinical Research and Special Projects at NIAID, and Vittorio Gallo, Ph.D., Interim Chief Academic Officer at Children’s National and Interim Director of the Children's National Research Institute, holds the mission to generate and apply knowledge to promote the prevention, diagnosis, treatment, and cure of these childhood diseases through its work together.
For each area, designated investigators from each institution are collaborating to design and conduct clinical research studies that will advance prevention strategies, diagnoses, treatments, and cures for the diverse range of pediatric diseases involving the immune system. Many of these studies will include children at high risk for complications related to their underlying disease or to experimental therapeutics and diagnostic tests they receive. Research participants will have the opportunity to be seen at both Children’s National and the NIH Clinical Center in Bethesda, Maryland. Together, the two institutions provide comprehensive, state-of-the-art pediatric clinical support, infrastructure, and research capacity. These resources protect the safety of children, ensure that they receive the highest quality of care, and offer them the opportunity to participate in cutting-edge clinical research. In addition, the partnership established joint training opportunities for physician-scientists interested in caring for these children while developing their research expertise in pediatric immunology, allergic, and infectious diseases.
Annual Children's National - NIAID Symposium
- 2022 Symposium
-
5th Annual Symposium (Virtual): June 2-3, 2022 | Recordings
This two-day symposium brought together investigators, researchers, and clinicians from National Institute of Allergy and Infectious Diseases (NIAID) and Children’s National Hospital as well as other interested participants from outside institutions, and discussed the creation, progress, and evolution of this first-of-its-kind collaboration between the NIAID at the National Institutes of Health and Children's National, a leading pediatric health system in the Washington, D.C., area.
This year's symposium highlighted the current COVID-19 and Autoinflammatory/Neuroimmune diseases, with the onsite location at the Children’s National Research and Innovation Campus in DC.
- 2021 Symposium
-

4th Annual Symposium (Virtual): June 3-4, 2021 | Recordings
This annual symposium celebrates the partnership between Children’s National Hospital (CNH) and the National Institute of Allergy and Infectious Diseases (NIAID). Established in 2017, the CNH-NIAID partnership focuses on advancing the health of children with allergic, immunologic, and infectious diseases through collaborative research and education.
In 2021, the Symposium was held on Thursday, June 3rd and Friday, June 4th as a virtual event that highlighted research on COVID-19 and multisystem inflammatory syndrome in children (MIS-C), and the intersectionality of COVID-19, allergy, and immunology on the pediatric population. Keynote speaker pediatric neurologist and 73rd Governor of The Commonwealth of Virginia, Ralph Northam, spoke on the COVID-19 pandemic and strategies to reintroduce children into schools and sports.
- 2020 Symposium
-

3rd Annual Symposium (Virtual): September 29, 2020 | Recordings
This year's symposium highlighted the latest COVID-19 and MIS-C pandemic, with a specific focus on the pediatric population. Dr. Anthony Fauci provided an overview on the infectious disease, and leading experts from Children's National, NIAID, and other institutions shared novel research and science being done to address this worldwide issue.
- 2019 Symposium
-
2nd Annual Symposium (NIH Natcher Conference Center | Bethesda, MD): November 8, 2019
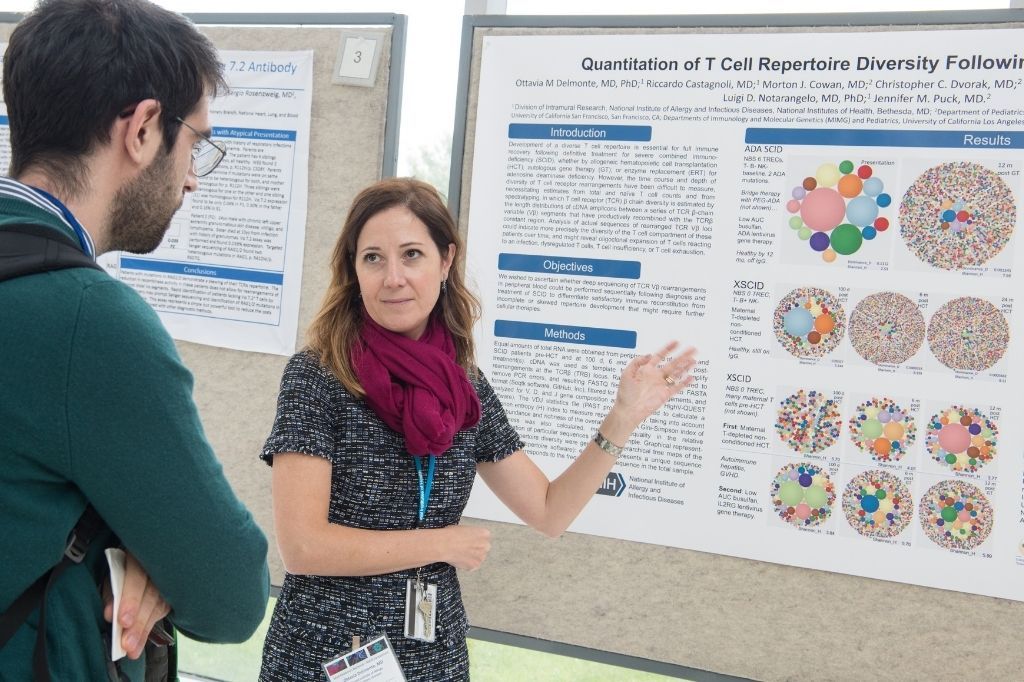
The 2nd annual Children’s National-NIAID Symposium presented outstanding research related to the partnership, including discussions on genomics, hereditary disorders, and gene therapies, by speakers from several NIH institutes and Children’s National, which included a poster session in the afternoon. Through this symposium, the partnership is committed to clinical and translational research and excellence in clinical care for children.
- 2018 Symposium
-
Inaugural Symposium (Children's National Hospital | Washington, DC): September 18, 2018
This one-day symposium brought together investigators, researchers, clinicians, and other interested participants from NIAID and Children’s National Hospital and discussed the creation, progress, and evolution of this first-of-its-kind collaboration between the NIAID at the National Institutes of Health and Children’s National Hospital, a pediatric academic medical center.
The symposium aimed to enhance knowledge and inspire present and future investigators to continue the search for innovative treatment approaches that will improve the lives of children with immunologic, allergic, auto-inflammatory, and infectious diseases.
Projects
- Primary Immunodeficiency Program
-
Protocol Title: Investigating the Mechanistic Biology of Immunodeficiency Disorders
This study investigates novel forms of primary immunodeficiency (PID) and to better define the natural history of both new and previously described forms of PID, including severe combined immunodeficiency (SCID), combined immunodeficiency, natural killer (NK) cell deficiency, and other disorders. Patients with clinical and/or laboratory evidence of PID will be recruited at Children's National and NIAID, and will provide one or more blood donations during the course of the study to enable immunologic and genetic investigations of immune pathways contributing to PIDs. These subjects will also be followed clinically to longitudinally assess the natural history of novel and known PIDs. Subjects will be followed over time with regard to their immunologic phenotype, clinical disease (including incidence of infections, autoimmune phenomena, allergic disease, or malignancies), and response to both preventative and definitive therapies. Biological relatives who do not have PID and healthy adult volunteers will also be eligible to serve as controls for this study.
Children's National

Vanessa Bundy, M.D., Ph.D., is an immunologist at Children’s National Hospital in Washington, D.C. She recently joined Children’s National from the University of California, Los Angeles (UCLA), where she completed fellowship training and was a clinical instructor. Dr. Bundy joins Children’s National as an Assistant Professor in the Allergy and Immunology Division. She is a member of the American Academy of Allergy, Asthma, and Immunology, the American College of Allergy, Asthma and Immunology and the Clinical Immunology Society. Her clinical interests focus on the diagnosis and treatment of recurrent infections and primary immune deficiency.

Michael Keller, M.D., is a pediatric immunologist at Children's National Hospital and specializes in the diagnosis and treatment of primary and secondary immunodeficiency disorders. He has authored many peer-reviewed articles and contributed to expert consensus guidelines on the treatment and diagnosis of primary immunodeficiency disorders. Dr. Keller is a member of the American Academy of Allergy, Asthma, and Immunology (AAAAI); the Clinical Immunology Society; the European Society of Immunodeficiency; and the Primary Immunodeficiency Treatment Consortium (PIDTC).
Dr. Keller's research focuses on the use of adoptive T-cell therapies for treatment of infections in immunocompromised patients, including the use of this therapy to improve outcomes in children with primary immunodeficiency disorders as well as those undergoing bone marrow transplantation for cancer. He is the primary investigator of several Phase I-II studies of virus-specific T-cell immunotherapy.
NIAID
Luigi D. Notarangelo, M.D. received his medical degree from the University of Pavia, Italy. After completing training in pediatrics, subspecialty training in allergy/immunology, and human genetics at the University of Pavia and a postdoctoral internship with David Nelson, M.D., at the Metabolism Branch, National Cancer Institute, he was appointed associate professor and subsequently full professor of pediatrics at the University of Brescia, Italy, where he chaired the department of pediatrics between 2000 and 2006. In November 2006, he joined the division of immunology at Boston Children’s Hospital, Harvard Medical School, as professor of pediatrics. In October 2016, he joined the Laboratory of Host Defenses.
Dr. Notarangelo is a leader in the study of the molecular and cellular mechanisms of human primary immune deficiencies and in the treatment of these disorders. He has served as president of the European Society for Immune Deficiencies and of the Clinical Immunology Society. He has received numerous national and international awards.
Ottavia Delmonte, M.D., is the Assistant Research Physician of the Clinical Immunology and Microbiology Laboratory at NIAID.
- Food Allergy Program
-
Protocol Title: Natural History and Mechanistic Investigation of Atopic Disease in Childhood
The prevalence of atopic and allergic diseases has increased both in developed and developing countries in recent decades. Atopic diseases typically manifest in early childhood, progress through the first decade of life through what has become known as the ‘atopic march’ and then often persist throughout one’s lifetime. This study will investigate the natural history of a/the peanut allergy in a cohort of food-allergic and food-sensitized infants and determine whether allergy and sensitization is attributable to differences in regulatory T and B cell frequency/function compared with non-allergic, age-matched controls.
Children's National

Hemant Sharma, M.D., M.H.S., is the Chief of the Division of Allergy and Immunology at Children’s National. He is an Associate Professor of Pediatrics at George Washington University School of Medicine, and the Director of the Food Allergy Program at Children’s National. He has served as the site director of the allergy immunology fellowship program with the National Institutes of Health. He is Director of the FARE (Food Allergy Research & Education) Clinical Network site at Children’s National.
He joined the faculty at Children’s National in 2008. His areas of clinical, advocacy and research interest include racial and socioeconomic health disparities and community-based management of food allergy. He writes a quarterly column in Allergic Living magazine and answers readers’ food allergy questions. He is heavily involved in advocacy, participating in regional and national legislative efforts to improve the health of the food allergy community. Dr. Sharma is board-certified in Pediatrics and in Allergy and Immunology, and is a fellow of the American Academy of Allergy, Asthma and Immunology, serving on the Adverse Reactions to Foods Committee. Due to his efforts on behalf of the food allergy community, he was selected to receive the 2016 FARE Vision Award.

Adora Lin, M.D., Ph.D., is a pediatric allergist at Children's National Hospital. Her research focuses on the regulation of B cells and immunoglobulin production during the development of food allergy and tolerance to foods. She also investigates regulatory B cells in healthy children and those with allergic diseases. Dr. Lin's primary goal is to elucidate the mechanisms underlying the development of food allergy vs. tolerance and to leverage these findings toward improved diagnosis, treatment, and prevention of food allergy and other allergic diseases.
NIAID

Pamela Guerrerio, M.D., Ph.D., graduated with a B.S. degree in biology from the University of Iowa and entered the Medical Scientist Training Program at Johns Hopkins University, where she completed medical school and a Ph.D. in human genetics. She also did her residency in pediatrics and fellowship in allergy and immunology at Johns Hopkins, and subsequently joined the faculty. In 2014, Dr. Guerrerio was recruited to the NIAID intramural research program as Chief of the Food Allergy Research Unit. She received tenure in 2019 and was named Chief of the Laboratory of Allergic Diseases in 2020. Dr. Guerrerio was the recipient of the ARTrust Faculty Development Award from the American Academy of Asthma, Allergy and Immunology in 2011. She received the Presidential Early Career Award for Scientists and Engineers, the National Science Foundation’s highest honor for science and engineering professionals in the early stages of their independent research career, in 2017.
- Infectious Disease Program
-
Protocol Title: Characterization of Pediatric Lyme Disease: Clinical Manifestations, Long Term Outcome, Immune Response, and Prevalence of PTLDs
The protocol proposes two paired substudies designed to characterize the clinical manifestations and long-term outcomes among pediatric Lyme disease patients in the greater Washington, DC area. Substudy 1 will characterize the natural history and longterm clinical, quality of life, and cognitive outcome of pediatric patients diagnosed with early and late stage Lyme disease, including prevalence of Post-Treatment Lyme Syndrome (PTLDS) and Substudy 2 will compare clinical, behavioral, cognitive and(future) immunologic response profiles between patients with full recovery, PTLDS and healthy controls. We will assess timeframe for resolution of symptoms after appropriate treatment, estimate the prevalence of PTLDS among a diverse cohort of pediatric patients diagnosed with Lyme disease within the past decade, and obtain specimens for future studies to identify the immune response of patients with PTLDS compared to patients who fully recovered from Lyme disease and healthy controls, as well as recently diagnosed patients with different manifestations of Lyme disease (early localized, disseminated, and late disease). Results of these analyses will be used to identify profiles and biomarkers that correlate with the outcome phenotypes. This signature could allow the design of a prognostic/diagnostic biomarker assays for patients with Lyme disease and PTLDS.
Children's National

Roberta L. DeBiasi, M.D., M.S., is Chief of the Division of Pediatric Diseases and Co-Director of the Congenital Zika Program at Children’s National Hospital. She holds appointments as tenured Professor of Pediatrics and Microbiology, Immunology and Tropical Medicine at George Washington University School of Medicine & Health Sciences as well as Principal Investigator in the Center for Translational Research at Children’s National Research Institute. Dr. DeBiasi’s research expertise includes basic science as well as clinical/translational research. She serves as Principal Investigator for research and clinical trials focusing on severe and emerging viral infections affecting pregnant women, neonates, immunocompromised hosts, and normal children. She is Co- Director of the Congenital Zika Program at Children's National which includes research protocols in the US and Colombia focused on prenatal imaging, testing, genetics and virologic aspects of congenital Zika infection. She leads the Children's National Ebola response and is Co-PI for federal funding to support Ebola preparedness. In addition, Dr. DeBiasi’s research portfolio includes a study evaluating the burden of pediatric Lyme disease, as well as long-term outcomes of Lyme infection in children. She is also involved in emergency investigational new drug (IND) acquisition of agents for treatment of severe viral myocarditis, encephalitis, and malaria. She is site PI for a PCORI- funded multicenter clinical trial evaluating optimal management of refractory Kawasaki Disease.
NIAID

Adriana Marques, M.D., is the Chief of the Lyme Disease Studies Unit, Laboratory of Clinical Immunology & Microbiology at the NIAID.
Protocol Title: Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study
The protocol is a multisite prospective observational study to evaluate the clinical sequelae of symptomatic and asymptomatic severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in the pediatric population, including coronavirus disease 2019 (COVID-19) and multisystem inflammatory syndrome in children (MIS-C), and characterize the immune response associated with these clinical presentations. Participants aged 21 years and younger with laboratory confirmed history of symptomatic or asymptomatic SARS-CoV-2 infection will visit the study sites for clinical and research evaluations and sample collection at schedules dependent on time since infection. Participants enrolled within 12 weeks after acute infection or positive test will be part of the “recovery group” and will attend study visits at baseline, every 3 months for the first 6 months, and subsequently every 6 months for a total of 3 years. Participants enrolled more than 12 weeks after acute infection or positive test will be in the “convalescent group” and will attend study visits at baseline and subsequently every 6 months for a total of 3 years.
Individuals (aged ≤21 years) without a diagnosis of SARS-CoV-2 infection or current symptoms suggestive of COVID-19 will serve as a control group and will attend visits for evaluations and sample collection at baseline and every 12 months for a total of 3 years. This protocol will establish a cohort of pediatric patients recovered from SARS CoV-2 infection and a biorepository for evaluation of the potential roles of host genetics, immune response, and other possible factors influencing long-term outcomes.
Children's National

Roberta L. DeBiasi, M.D., M.S.
NIAID

- Neuro-Immune Program
-
Protocol Title: Natural History Study of Pediatric-Onset Neuro-Immune Conditions with Discovery of Dysregulated Molecular And Genetic Pathways (NI-MAP)
A natural history protocol for the evaluation of patients with genetically defined or undifferentiated pediatric diseases characterized by inflammation of the central nervous system using advanced genetics and immunophenotyping is currently being developed. Affected participants will be clinically evaluated and provide biological samples for research. Leftover samples from clinical procedures may also be used for research. Genotyping, HLA typing and immunophenotyping will be performed free of charge. Follow-up visit may be scheduled on the basis of clinical status, with the aim of molecularly characterizing biologic samples including CSF in both active and quiescent states. Unaffected biological parents will provide biological samples to be used as controls.
Children's National

Elizabeth Wells, M.D., is a graduate of Harvard University and the George Washington University School of Medicine and Health Sciences. She holds a master’s in Health Science from the NIH/Duke Clinical Research Training Program. Dr. Wells completed her pediatrics and neurology training at Children’s National Hospital and has been on staff as a pediatric neurologist within the Brain Tumor Institute and the Division of Neurology for the past 10 years.
In addition to her work in neuro-oncology at Children’s National, Dr. Wells also developed the multidisciplinary program in pediatric neuro-immunology. She serves on numerous national committees and receives national and international referrals for children with neuro-inflammatory disorders. She is a principal investigator for translational research studies and serves in a leadership role for the Clinical and Translational Science Institute at Children's National and the District of Columbia Intellectual and Developmental Disabilities Research Center. Dr. Wells has been director of Inpatient Neurology and the Neuroscience medical unit director since 2015 and was elected president of the medical staff in July 2020. In her role as vice president, Dr. Wells focuses on the programmatic development of the Center including work on quality and safety, medical informatics, diversity and inclusion and patient experience.

Ilana Kahn, M.D., is the Clinical Director of Neuroimmunology and the Director of the Pediatric Multiple Sclerosis Options at Children's National Hospital.
NIAID

Raphaela T. Goldbach-Mansky, M.D., M.H.S., received her medical degree from the University Witten-Herdecke, Germany, in 1990 and completed a combined residency in internal medicine and pediatrics at Case Western Reserve University, Metro Health Medical Center. She completed her rheumatology fellowship training at NIAMS in 1999 and served as a staff clinician at NIAMS through 2008. Dr. Goldbach-Mansky is chief of the NIAID Translational Autoinflammatory Disease Studies (TADS) Unit. She leads the NIAID autoinflammatory disease clinic and has built a translational research program focusing on clinical and translational studies in children with early-onset autoinflammatory diseases. Together with Dr. Daniel Kastner (NHGRI) she founded the Translational Autoinflammatory Research Initiative (TARI) at NIH to improve research in patients with rare autoinflammatory diseases.
Dr. Goldbach-Mansky's research focus is on applying a systematic approach to the clinical and immunological study of autoinflammatory diseases. Her group uses targeted interventions to understand the role of specific inflammatory pathways in the pathogenesis of autoinflammatory diseases.

Bibi Bielekova, M.D., received an M.D. in 1993 from Comenius University in Bratislava, Slovakia. After a medical internship at SUNY Downstate Medical Center in Brooklyn and a neurology residency at Boston University, she did a 3-year postdoctoral research fellowship at the NINDS Neuroimmunology Branch (NIB). She remained at NIB for an additional 5 years as a staff physician, focusing on development of novel therapies for MS. In 2005, she became associate professor of neurology with tenure and director of the Waddell Center for MS at University of Cincinnati. In 2008, she moved back to NINDS as an investigator. In 2018, Dr. Bielekova transferred as a senior investigator to NIAID. Her laboratory is studying mechanisms of immunoregulation and immune-mediated CNS tissue injury in MS and other neuroimmunological diseases with a long-term goal of developing effective therapies. In addition, Dr. Bielekova is a principal investigator on several innovative protocols including adaptively designed Phase I/II clinical trials.
- Fellowship Training Program
-
One of the overarching goals of the CNH-NIAID partnership is to provide joint training opportunities for investigators studying and caring for children with infectious, immunologic, and allergic diseases. To date, 12 exceptional fellows have matched and been placed into the training programs. In 2020, a formal career mentorship program and a protocol writing workshop with program officers from the NIH Division of Allergy, Immunology, and Transplantation (DAIT) was initiated to better prepare fellows for careers in academic medicine
Children's National

Suzanne Kochis, M.D., is the site director of the National Institute of Allergy and Infectious Diseases allergy and immunology fellowship program. She completed pediatric allergy immunology fellowship training at Johns Hopkins University. She obtained her M.D. from Jefferson Medical College of Thomas Jefferson University and then completed pediatric residency at Johns Hopkins, where she also served as Chief Resident. Her research at Hopkins focused on parental understanding of pediatric asthma control and outcomes for asthma, as well as a quality improvement project assessing adrenal insufficiency in patients with eosinophilic esophagitis on swallowed topical steroids. She now specializes in food allergies.
Dr. Kochis was the recipient of the American Academy of Pediatrics (AAP) Section on Allergy and Immunology (SOAI) Outstanding Abstract Award in 2017. She completed a Certificate in Quality, Patient Safety and Outcomes Research at the Johns Hopkins Bloomberg School of Public Health.

Nada Harik, M.D., is an attending physician in the Division of Infectious Diseases at Children's National Hospital in Washington, D.C and an Associate Professor of Pediatrics at the George Washington University School of Medicine and Health Sciences.
Dr. Harik is the director of the Pediatric Infectious Diseases Fellowship Program at Children's National. She also serves as the clinical consultant for the Infection Control Program. Her main research and clinical interests are Staphylococcus aureus epidemiology and pathogenesis, osteomyelitis/septic arthritis, infections in children with cystic fibrosis, infection prevention, tick-borne infections, medical student/resident/fellow education and pediatric tuberculosis. Dr. Harik is an active member of the Pediatric Infectious Diseases Society.
NIAID

Paneez Khoury, M.D., M.H.Sc., FAAAAI, is an associate research physician at NIAID. She has been involved in translational research in eosinophilic disorders since joining the Human Eosinophil Section in 2012.She received her M.D. from University of Illinois College of Medicine in Chicago. She completed an internal medicine residency at the Ohio State University followed by a fellowship in allergy and clinical immunology at NIH. She also holds a master’s of health sciences from Duke University. She is board certified in internal medicine and allergy/immunology and is a fellow of the American Academy of Allergy, Asthma and Immunology (AAAAI).
At NIH, she serves as the chair of the Scientific Review Committee of the Laboratory of Parasitic Diseases. She sits on the graduate medical education (GME) committee, including the policy subcommittee, and is a member of the staff clinician council. Her external committee activities include involvement in the food allergy and eosinophilic disorders committee, the program directors assembly, and the leadership institute of AAAAI . She serves on the board of the International Eosinophil Society (IES) and is the social media chair for the society.
Leadership
- Governing Board
-

Vittorio Gallo, Ph.D., is interim chief academic officer at Children’s National Hospital and interim director of the Children's National Research Institute (CNRI). As an internationally renowned neuroscientist, Dr. Gallo previously served as director of the Children’s National Center for Neuroscience Research for a decade. He is the Wolf-Pack Chair in Neuroscience within CNRI. In his current position as Interim Chief Academic Officer, Interim Director of the Children's National Research Institute and Associate Dean at GWU, he continues his efforts in promoting translational research and enhancing integration between lab-based and clinical investigation at the two institutions. He also continues to play a major mentorship role for both junior faculty, clinician scientists and fellows, many of them supported by career development awards.

H. Clifford Lane, M.D. serves as the National Institute of Allergy and Infectious Diseases' (NIAID) Deputy Director for Clinical Research and Special Projects. Dr. Lane's responsibilities include directing the activities of the Division of Clinical Research, which supports both intramural and extramural research involving human volunteers
- Executive Steering Committee
-

Catherine Bollard, M.D., M.B.Ch.B., is the Director of the Center for Cancer and Immunology Research at the Children’s National Research Institute, Director of the Program for Cell Enhancement and Technologies for Immunotherapy and a member of the Division of the Blood and Marrow Transplantation. In addition, she is a Professor of Pediatrics and Microbiology, Immunology and Tropical Medicine at the George Washington University and is the ACD for Translational Research and Innovation within the George Washington Cancer Center. In these roles, Dr. Bollard leads clinical and research efforts to fight cancer and other inflammatory diseases by strengthening the immune system using adoptive cell therapy. As a past president of the International Society of Cellular Therapy, and the current president of the Foundation for the Accreditation for Cellular Therapy (FACT) she is a distinguished hematologist, immunologist and immunotherapist, working to develop cell and gene therapies for patients with cancer and underlying immune deficiencies.
Jeffrey Dome, M.D., Ph.D., is Senior Vice President of the Center for Cancer and Blood Disorders and Chief of the Division of Oncology at Children’s National Hospital in Washington, D.C. He also is Professor of Pediatrics at the George Washington University School of Medicine & Health Sciences and the Thomas Willson and Lenore Williams McKnew Professor of Pediatric Oncology. Dr. Dome received his M.D. degree from the University of Pennsylvania School of Medicine and his Ph.D. degree in Medicine from Erasmus University in Rotterdam. He completed a residency in Pediatrics at Yale-New Haven Hospital and a fellowship in Pediatric Hematology/Oncology at Johns Hopkins Hospital. After fellowship, Dr. Dome was a faculty member at St. Jude Children’s Research Hospital before joining Children’s National Hospital in 2006. Dr. Dome is an internationally recognized expert on pediatric solid tumors, with an emphasis on kidney tumors and sarcomas. He chaired the Children’s Oncology Group (COG) Renal Tumor Committee, which oversees clinical research on kidney tumors at more than 200 children’s hospitals around the world, for more than 10 years. Dr. Dome is the Continental President of North America for the International Society of Paediatric Oncology (SIOP). He is a member of the Hematology/Oncology Sub board of the American Board of Pediatrics and serves on numerous medical advisory boards for cancer foundations. He has authored more than 150 articles, books and chapters on pediatric cancer.

Lisa M. Guay-Woodford, M.D., is the Richard L. Hudson Professor of Pediatrics at Children’s National Hospital and the George Washington University School of Medicine & Health Sciences (GW). She also serves as the associate vice president for Clinical and Translational Research at GW. She has become an internationally recognized pediatric nephrologist with a research program focused on identifying clinical and genetic factors involved in the pathogenesis of inherited renal disorders, most notably autosomal recessive polycystic kidney disease (ARPKD). In addition to her clinical and investigative work, Dr. Guay-Woodford has been a leader in promoting clinical and translational science. She established the UAB Hepato-Renal Fibrocystic Disease Research and Translational Core Center, funded by a National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) P30 award. She was the founding Director of the UAB Center for Clinical and Translational Science, funded by the National Institutes of Health (NIH) Clinical and Translational Science Award (CTSA) program. Currently, she serves as Director of the Children’s National Research Institute Center for Translational Research, as well as Director of the Clinical and Translational Science Institute at Children’s National (CTSI-CN), which is also funded by the NIH CTSA program.

Pamela Guerrerio, M.D., Ph.D., graduated with a B.S. degree in biology from the University of Iowa and entered the Medical Scientist Training Program at Johns Hopkins University, where she completed medical school and a Ph.D. in human genetics. She also did her residency in pediatrics and fellowship in allergy and immunology at Johns Hopkins, and subsequently joined the faculty. In 2014, Dr. Guerrerio was recruited to the NIAID intramural research program as Chief of the Food Allergy Research Unit. She received tenure in 2019 and was named Chief of the Laboratory of Allergic Diseases in 2020. Dr. Guerrerio was the recipient of the ARTrust Faculty Development Award from the American Academy of Asthma, Allergy and Immunology in 2011. She received the Presidential Early Career Award for Scientists and Engineers, the National Science Foundation’s highest honor for science and engineering professionals in the early stages of their independent research career, in 2017.

Gina Montealegre, M.D., is a physician scientist within the Division of Clinical Research, NIAID. She is a pediatric rheumatologist with a master's degree in Clinical Research. Dr. Montealegre has an extensive background in the development, execution and oversight of clinical trials in rare autoinflammatory diseases. Previously, she worked as a director of the Clinical Trials Unit at the Translational Autoinflammatory Disease Section at NIAID.
Luigi D. Notarangelo, M.D., received his medical degree from the University of Pavia, Italy. After completing training in pediatrics, subspecialty training in allergy/immunology, and human genetics at the University of Pavia and a postdoctoral internship with David Nelson, M.D., at the Metabolism Branch, National Cancer Institute, he was appointed associate professor and subsequently full professor of pediatrics at the University of Brescia, Italy, where he chaired the department of pediatrics between 2000 and 2006. In Nov. 2006, he joined the division of immunology at Boston Children’s Hospital, Harvard Medical School, as professor of pediatrics. In Oct. 2016, he joined the Laboratory of Host Defenses.
Dr. Notarangelo is a leader in the study of the molecular and cellular mechanisms of human primary immune deficiencies and in the treatment of these disorders. He has served as president of the European Society for Immune Deficiencies and of the Clinical Immunology Society. He has received numerous national and international awards.

David Wessel, M.D., is executive vice president, chief medical officer, physician-in-chief and the Ikaria Distinguished professor of Critical Care Medicine at Children's National Hospital. He is also professor of anesthesiology, critical care medicine and pediatrics at the George Washington University.
Dr. Wessel is internationally known for his pioneering work in caring for infants with heart disease. An experienced scientist and clinical researcher with more than 100 peer-reviewed publications, Dr. Wessel has designed and executed seminal studies in cardiac critical care and pulmonary hypertension; developed new therapies for perioperative care of the newborn with congenital heart disease and novel treatments of pulmonary hypertension; and studied neurologic outcomes relevant to perioperative care of newborns with congenital heart disease. He is a principal investigator and member of the steering committee for the Collaborative Pediatric Critical Care Research Network sponsored by the National Institutes of Health.
- Program Director
-

Helen Kim, MBA, serves as the Program Director for the Children's National Hospital-National Institute of Allergy and Infectious Diseases partnership. She has a Master’s degree in Business Administration from the Johns Hopkins Carey Business School. As Program Director, Helen provides leadership and oversight for all aspects of the collaborative partnership between the two institutions. Prior to joining Children's National, she was the Senior Clinical Research Program Manager in the Department of Radiation Oncology and Molecular Radiation Sciences at Johns Hopkins.
- Operations
-

Stephanie Norman, M.P.H., joined the Children's National-NIAID partnership in July 2019 as the Clinical Research Coordinator. She has a Master's degree in Public Health from New York University. Prior to working at Children's National Hospital, she was a Clinical Research Coordinator in Maternal Fetal Medicine at Mount Sinai Hospital in New York City. AS the coordinator for the partnership, she works on regulatory submissions, data entry, recruitment and enrollment as well as other tasks associated with daily protocol activity.
Christine Peng, B.S.N, B.S., R.N., is the Research Nurse for the Children's National-NIAID partnership. Seh received her B.S. degree in Behavioral and Community Health from the University of Maryland, College Park, and B.S. in Nursing from University of Maryland, Baltimore. Christine's roles within the partnership include providing education and support for the clinical research studies and functioning as a resource for the Principal Investigators, patient/family, and community.
Infectious Disease Program: Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study

Saira Huq, M.P.H., is the Project Manager for the Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study. She has a Master of Public Health degree from the University of Pennsylvania and is a Fulbright Scholar. Prior to joining Children’s National, she helped evaluate federally funded public health programs and clinical trials at NORC at the University of Chicago and Westat. As project manager she coordinates study activities, monitors study progress, reports to the study sponsor, and helps ensure that project activities are completed on time, on budget, and within scope.

Lauren Arrigoni, C.P.N.P., R.N., is the pediatric nurse practitioner (NP) for the Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study with the Children's National-NIAID partnership. Her previous roles include pediatric heart transplant NP and Pediatric ICU nurse in NYC. At the height of the COVID-19 Pandemic in NYC in 2020, she was redeployed as a bedside nurse for the pediatric COVID-19 Unit and followed discharged COVID-19 pediatric patients as a part of the cardiology team.
She is completing her Doctor of Nursing Practice at the University of Pennsylvania. She obtained her BSN from the University of Pennsylvania as a Hillman scholar. While working full-time in the PICU, she graduated as a Pediatric Nurse Practitioner from NYU where she was given the Rising Star Award. She also volunteers as a camp nurse at the Double H Ranch, which is a camp for children with serious and chronic illnesses, founded by Paul Newman. She has volunteered with MakerNurse, a group supporting nurse innovations and served as a guest of Doctor Radio on SiriusXM. Lauren’s roles within the study include conducting study visits, assessing study test results, and enrolling participants for the study.

Mallory Barrix, M.P.H., C.H.E.S., joined the Children’s National-NIAID partnership in June 2021 as a Clinical Research Coordinator on the Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study. She has a Bachelor of Science in Human Development and Family Studies from the University of Wisconsin- Madison as well as a Master of Public Health degree from Emory University. In addition, she is also a Certified Health Education Specialist. As a Coordinator for the Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study, she handles regulatory submissions, patient recruitment and enrollment, and study visit organization among other tasks aimed at helping the study run smoothly.

Maureen Edu, B.S., began working as a clinical research coordinator for the Pediatric SARS-CoV-2 and MIS-C Long-term Follow-up Study in January 2022. She assists with enrollment, recruitment, regulatory submission, data collection/entry, and other daily operations of the clinical study. She obtained her B.S. in Biology from Randolph College. She formerly worked as a research coordinator for the Center for Prevention and Early Intervention at the Johns Hopkins Bloomberg School of Public Health.
WELCOME TO THE
6th Annual Children's National Hospital - NIAID Symposium
Promoting Child Health: From Environmental Challenges to Pandemic
April 27 - 28, 2023 | Children's National Research and Innovation Campus | 7144 13th Pl NW, Washington, DC 20012
This annual symposium celebrates the partnership between Children’s National Hospital and the National Institute of Allergy and Infectious Diseases (NIAID). Established in 2017, the Children's National - NIAID partnership focuses on advancing the health of children with allergic, immunologic, and infectious diseases through collaborative research and education.
This year’s hybrid event will be held on Thursday, April 27th and Friday, April 28th, 2023 at the Children’s National Research and Innovation Campus in DC. Together with our co-host, the Pediatric Pandemic Network (PPN), we will focus on Promoting Child Health: From Environmental Challenges to Pandemic.
The Pediatric Pandemic Network is a network of 10 children’s hospitals that serve as regional hubs for improving care for all children, their families, and communities in pandemics, disasters and every day. The PPN works with regional and national programs, academic institutions, community organizations, and individual experts to share pediatric-related information, educational resources, and best practices. In 2023, the priority focus areas for PPN activities include infectious disease/disease outbreaks, mental and behavioral health, healthcare emergency management, and health equity and community engagement.
Funding for this event has been provided by Children's National Research Institute, Center for Cancer and Immunology, and Center for Translational Research.
SYMPOSIUM RECORDING
- Day 1, Thursday, April 27, 2023 | View video recordings
- Day 2, Friday, April 28, 2023 | View video recordings
AGENDA
THURSDAY, APRIL 27, 2023 | Environmental Challenges to Child Health |
||
| Welcome |
|
|
|
12:00 - 12:30 pm |
|
Keynote Presentation |
|
"Tropical Medicine Vaccine Sciences to Catalyze Global Child Health" Maria Elena Bottazzi, PhD, FASTMH
|
||
|
12:30 - 2:30 pm |
Session 1: Environmental Factors and Impact on Allergy
|
|
| 12:30 - 12:55 pm |
“Evaluating Air Pollution as a Driver of Atopic Dermatitis"
|
|
| 12:55 - 1:20 pm |
"Environmental Factors Contributing to the Food Allergy Epidemic"
|
|
| 1:20 - 1:45 pm |
"Childhood Asthma and Urban Environmental Exposures: Challenges and Possible Solutions"
|
|
| 1:45 - 2:10 pm |
Roundtable Q&A
|
|
| 2:10 - 2:20 pm |
Abstract Presentation: "ROSAH: A New Dominantly Inherited Disease Causing Autoinflammation and Progressive Blindness"
|
|
| 2:20 - 2:30 pm |
Abstract Presentation: "The Intersection Between Asthma Morbidity and Healthy Housing" Creation of an Interactive Health Housing Map for the District of Columbia"
|
|
| 2:30 - 3:00 pm |
Break
|
|
| 3:00 - 5:00 pm |
Session 2: Environmental Impact on Infectious Diseases
|
|
| 3:00 - 3:35 pm | “Using a One Health Approach to Address the Planet’s Most Wicked Problems – Linked Health Risks Resulting From the Climate Crisis and Emerging Infectious Diseases”
Jonna Mazet, DVM, MPVM, PhD
|
|
| 3:35 - 4:10 pm |
"Syndemic Perspective on Prevention and Response: How the National Mpox Response Activated Close Friends and New Partners" |
|
| 4:10 - 4:40 pm |
"Flooding in Pakistan, Disease Outbreaks, and Climate Justice"
|
|
|
4:40 - 4:50 pm |
|
Abstract Presentation: "SARS-CoV-2 mRNA Vaccination Induces B cell Immunity in the Tonsils and Adenoids of Children"
|
| 4:50 - 5:00 pm |
Abstract Presentation: "Temporal Trends of Blood Glucose in Children with Cerebral Malaria"
|
|
| 5:00 pm |
Reception
|
|
FRIDAY, APRIL 28, 2023 | Pandemic Preparedness |
||
| Welcome |
Larry K. Kociolek, MD, MSCI, FSHEA, FPIDS
|
|
| 9:00 - 9:30 am | Keynote Presentation | |
|
"Pediatric Pandemics, Public Health Emergencies and Disasters: A Need for Capacity, Coordination and Science Across the Disaster Continuum"
|
||
|
9:30 am - 12:00 pm |
Session 1: Pandemic Policy
|
|
| 9:30 - 9:35 am |
"Overview of the History of Developing the Pediatric Pandemic Network"
|
|
| 9:35 - 10:00 am |
"The HRSA Pediatric Pandemic Network: Preparing for the Next Disaster"
|
|
| 10:00 - 10:30 am | "Pediatric Pandemic Network Preparedness and Responsiveness with a Community Engagement and a Health Equity Lens"
Tamera Coyne-Beasley, MD, MPH and Ariann Nassel, MA
|
|
| 10:30 - 11:00 am | "Looking Forward: Addressing the Mental Health Crisis in Children and Adolescents"
Lee S. Beers, MD |
|
| 11:00 - 11:30 am |
“Lessons Learned From the 2022 Pediatric Viral Respiratory Surge: The Intersections of Infectious Disease and Pediatric Emergency Management”
|
|
| 11:30 am - 12:00 pm |
Panel Discussion: Building Pediatric Capacity Solutions
|
|
| Closing |
Larry K. Kociolek, MD, MSCI, FSHEA, FPIDS |
|
This agenda may be subject to change. Please check back for updates or subscribe to the CTSI-CN newsletter to receive the latest information.
Questions? Contact us at CN-NIAIDPartnership [at] childrensnational [dot] org (CN-NIAIDPartnership[at]childrensnational[dot]org).
SPEAKERS

Distinguished Investigator |

Medical Director, Community Health and Advocacy |

KEYNOTE SPEAKER Associate Dean, National School of Tropical Medicine |

Derrol Dawkins MD Endowed Chair in Adolescent Medicine |

Deputy Coordinator |

MODERATOR Div. Chief, Infectious Diseases |

KEYNOTE SPEAKER Medical Officer |

Associate Professor of Pediatrics |

Attending Physician, |

SPONSOR SPEAKER |
MODERATOR Division Chief, Pediatric Emergency Medicine |

Chief Executive Officer |

Vice Provost – Grand Challenges
|

Staff Clinician, Epithelia Therapeutics Unit
|

Pediatric and Trauma Surgeon |
Assistant Professor of |

MODERATOR Division Chief, Allergy and Immunology |

Allergist |

Division Chief, Emergency Medicine |

Washington Correspondent, |
|
Accreditation Statement:
This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Medical Society of Virginia (MSV) through the joint providership of Inova Office of Continuing Medical Education and Children's National Medical Center. The Inova Office Continuing Medical Education is accredited by the Medical Society of Virginia to provide continuing education for physicians.
Credit Designation:
The Inova Office of Continuing Medical Education designates this live activity for a maximum of 7.5 AMA PRA Category 1 Credit(s) ™. Physicians should only claim credit commensurate with the extent of their participation in the activity. Physicians may claim up to 7.5 credits in Type 1 CME on the Virginia Board of Medicine Continued Competency and Assessment Form required for renewal of an active medical license in Virginia.
Inova Health System’s Office of Continuing Medical Education adheres to ACCME’s Standards for Integrity and Independence in Accredited Continuing Education. Any individuals in a position to control the content of a CME activity, including faculty, program directors, and planners are required to disclose all relevant financial relationships with ineligible entities as defined by ACCME.
Catherine Bollard, MD, MBChB, planner for this educational event, has honorarium relationship with Mana Therapeutics, Catamaran Bio, Cabaletta Bio; receipt of intellectual property rights relationship with Mana Therapeutics and Catamaran Bio; ownership relationship with Mana Therapeutics, Catamaran Bio, Cabaletta Bio; consulting relationship with Sobi, Pfizer, BMS, Cellectar. All relevant financial relationships listed for this individual has been mitigated.
Maria Elena Bottazzi, PhD, faculty for this educational event, has royalty relationship with Biological E BioFarma. All relevant financial relationships listed for this individual has been mitigated.
Tamera Coyne Beasley, MD, MPH, faculty for this educational event, has consulting relationship with Pfizer, Moderna, Sanofi Pasteur. All relevant financial relationships listed for this individual has been mitigated.
Ruchi Gupta, MD, faculty for this educational event, has contracted research relationship with Novartis; consulting relationship with Genentech, Novartis, Aimmune LLC, Allergenis LLC; ownership relationship with Yobee Care, Inc. All relevant financial relationships listed for this individual has been mitigated.
Larry Kociolek, MD faculty for this educational event, has contracted research relationship with Merck. All relevant financial relationships listed for this individual has been mitigated.
- Featured Abstracts
-
- Linda Herbert
Acceptability, Feasibility, and Initial Results from a Behavioral Intervention for Early Adolescents with Food Allergy: The Food Allergy Mastery Program - Christopher Cole Honeycutt
Hybrid Immunity Elicits Cross-Reactive Memory B Cells and Protects Against SARS-CoV-2 BA.1 Replication in Rhesus Macaques - Danielle Kristin Sohai
Safety and Antiviral Response Monitoring Post Infusion of Autologous HIV-Specific T Cells Targeting Conserved Epitopes in Individuals with HIV on Antiretroviral Therapy: A Phase I Clinical Trial (NCT03485963)
- Linda Herbert
- Abstracts
-
- Scott Call
Social Needs Screening in Critically-Ill Pediatric Patients with Asthma - Ilana Kahn
Initial Disease Severity Predicts Executive Functioning in Children with Anti-NMDA Receptor Encephalitis (NMDARE) - Alexandra B. Kornbluh
Cerebrospinal Fluid Eosinophils in Pediatric Myelin Oligodendrocyte Glycoprotein Antibody-Associated Disease (MOGAD) - Olufunke Y. Martin
The Evolution of the COVID-19 Pandemic in Pediatric Patients with Sickle Cell Disease: From Alpha to Omicron - Chase D. McCann
Phenotypic and Functional Impacts of Successive Antigen Stimulation on T cells: Implications for Clinical Manufacturing of TAA-T cell Products - Maryam A. Pasdar
Utilizing mRNA as a Source of Antigens for the Expansion of Virus-Specific T cells - Shilpa J. Patel
- Kazuhiro Sabet
Increased Proliferation and Specificity of Tumor Associated Antigen Specific T-cells Using Checkpoint Inhibitor During Stimulation - Jillian P. Smith
Immune Activation by Antigen-specific T Cells Elicited in Patients Receiving Standard Therapy for Pediatric Solid Tumors - Lani Tran
Zika Infection Dysregulates Autophagy in Neural Stem Cells - Meagan E. Williams
United States Neurodevelopmental Outcomes of Zika Virus-Exposed Preschoolers
- Scott Call
- When is the 2023 event?
-
Thursday, April 27th from 12:00 pm - 5:00 pm and Friday, April 28th from 9:00 am - 12:00 pm
- Where is the event held?
-
The Children’s National Hospital - NIAID Symposium will take place at the Children’s National Research & Innovation Campus, located at 7144 13th Pl NW, Washington, DC 20012. Presentations on Thursday and Friday will take place in the Conference Theater located adjacent to the parking garage. The wine & cheese reception on April 27th will be held on the second floor of the Atrium across the street
- Where should I park?
-
Navigate to the intersection of "Fern St, NW and 13th Place, NW". Do not use the building address, as GPS apps may direct you through the larger Walter Reed campus on roads that are not open. Turn south on 13th Place and immediately turn left into the parking garage. This is level 3. Park at the far end of the garage (the south end) on level 3 and use the south end stairs to exit on level 2. The Conference Theatre will be located on the same side of the street as the garage. There will be signage to direct you.
The parking garage has a maximum daily cost of $16; however, free parking vouchers will be provided for this event. Please indicate your need for a voucher during registration.
- Where can I register?
-
Registration is now open! In-person registration will close when the maximum capacity allowance has been reached. However, registration to attend virtually will remain open until the event is concluded.
- Is there a registration fee?
-
No. This event is free to attend!
- Will CME credits be offered?
-
Yes!
Claiming credit instructions:
You can claim 7.5 credits for this CME event by visiting the Inova CME System (ICMES). You will need to log in using your existing account or by creating a new account. Once logged in you will click on your “Dashboard” in the top left corner then within the first tile click on “Claim CME Active Credits”. If you do not immediately see “2023 Children's National Hospital-National Institute of Infectious Diseases (NIAID) Hybrid Symposium Co-hosted by the Pediatric Pandemic Network (PPN)” click on “Other Available Activities” or use the search field and search for the event title. To the right of the meeting name, click on “Claim” then “Add New”. There will be an evaluation to complete and then the opportunity to claim the credit and download the certificate.
The deadline to claim credit to May 25, 2023.
- What are the COVID-19 Operational Guidelines?
-
We will be adhering to the current Children’s National Safety Guidelines. Effective Monday, April 3, masks are no longer required at our facilities for employees/visitors (with few exceptions). Therefore, masks are optional, but welcome at this event.